What should I expect during rehabilitation for my elbow?
Nonsurgical Rehabilitation
The main goal of nonsurgical physiotherapy treatment at COMPHYSIO for OA in your elbow is to help you manage your pain, maintain your elbow range of motion and strength, and to teach you how to use your elbow without causing more harm.
During the first few appointments at COMPHYSIO your therapist will focus initially on relieving your pain. Your therapist may use modalities such as heat, ice, ultrasound, or electrical current to assist with decreasing any pain or swelling you have around your elbow or anywhere along the forearm, at the shoulder, or into your hand. Your therapist may also use massage directly around your elbow or for your neck, shoulder, forearm, or wrist to improve circulation, assist with the pain, and make moving your entire upper extremity easier. To assist in getting rid of your pain, you may also need to modify or limit your activities that irritate the elbow. Your physiotherapist will advise you on how best to do this.
Resting the joint can help ease pain and inflammation especially if the joint is very irritable. A relative rest, where certain irritating activities are limited but others are allowed, may be enough to calm the symptoms down. Your physiotherapist may also suggest that you use a special elbow splint to immobilize and protect the elbow. Taping the elbow may also provide some relief. Some patients with OA also find relief when they use a topical rub. Your physiotherapist can advise you on if there would be any benefits to using braces, taping, creams or rubs in your individual case.
Next your physiotherapist will prescribe a series of stretching and strengthening exercises for your elbow. If you have lost any range of motion (ROM) in your ability to bend, straighten, or rotate your elbow your physiotherapist will measure this. They will also measure your grip strength on both sides. ROM and grip strength measures are very useful in order to track improvements and to ensure that the elbow is not declining further in function. Depending on the progression of OA in your elbow, simply not having a decline in ROM or strength may be considered very successful rehabilitation. In other words, sometimes as long as your symptoms, ROM, and strength are not getting worse over time, even though they may not be getting better, rehabilitation can be deemed a success.
Several stretching exercises for your elbow will be prescribed. If you have lost some ROM these exercises will be used to assist in re-gaining this ROM. Usually full ROM will not be achieved if you have already lost a significant amount of motion, but improvements can most often be made. If you have not lost any ROM then the stretches are used to maintain your range, and also to maintain the length of the muscles that cross your elbow joint. Tight muscles can be detrimental to the joint as they add pressure to the articular cartilage inside. If needed, your physiotherapist will mobilize your elbow joint. This hands-on technique is used to encourage the elbow to move into its normal ROM. With OA, mobilizing the joint can be particularly useful. Sometimes gaining even just a few degrees of ROM allows you to use your elbow more easily and eases symptoms.
Next your physiotherapist will prescribe some strengthening exercises for your elbow. By maintaining the strength in the muscles surrounding your elbow, the pressure is minimized on the elbow joint. Strength in your wrist as well as in your shoulder and shoulder blade area are also important in order for the elbow to function optimally. The shoulder blade is the upper extremity’s link to the torso so strength and control of this area is particularly crucial in being able to stabilize the arm so that the elbow can work well. Gripping exercises, although done with the hand, primarily use the muscles of the forearm, which connect to the elbow and are therefore an important part of your rehabilitation program. You will be pleased when your grip strength improves as daily activities such as twisting door handles or pulling or lifting heavier items such as shopping bags will become easier and less painful.
The use of free weights or elastic bands may be incorporated into your exercise routine in order to build up the strength of the muscles supporting your elbow, shoulder, and wrist. As your elbow becomes strong, eccentric exercises will be added. Eccentric exercises are ones where weight is applied as the muscles are lengthening. An example of this is holding a weight in your hand and moving from a bent elbow position to a straight one. Eccentric exercises are crucial in preparing the muscles and tissues around the elbow joint to take the load of everyday activities, such as lifting a tea kettle up and then lowering it onto the stove. As you get even stronger, your physiotherapist will increase the speed of your strengthening exercises in order to further build up the strength and more closely simulate the every day activities your elbow will be required to perform.
Exercises to improve your proprioception will also be added. Proprioception is the ability to know where your body is without looking at it. Receptors in your joints and ligaments primarily control proprioception so an injury to the joint will have a significant impact on one’s proprioception. Any period of immobility of the joint will add to this decline. Even activities such as assisting yourself with your arms to get out of a chair, pulling a glass from a cupboard, lifting a pot, or pushing a door open requires weight to be transmitted through your elbow and for your body to be proprioceptively aware of your limb. Participating in sporting activities with your upper extremity requires an even higher level of proprioceptive control. For this reason, proprioceptive exercises will be an important part of your rehabilitation regime at COMPHYSIO and your physiotherapist will be strict about your technique with these exercises in particular. As mentioned above these exercises will also include ones for the shoulder and shoulder blade, which is the elbow’s link to the torso. Proprioceptive exercises might include activities such as rolling a ball on a surface with your hand, holding a weight up overhead while bending and straightening your elbow, or push-ups on an unstable surface. Advanced exercises may include activities such as throwing or catching a ball.
In order to reduce your pain or assist with the biomechanics of your elbow joint, your physiotherapist may use some tape on your elbow. In some cases this can be quite useful to decrease your pain, which then allows you to strengthen the joint more easily. The tape can also allow you to do more everyday activities without discomfort. Some braces for the elbow can do the same thing. Your physiotherapist will advise you if taping or bracing may be useful in your situation.
We highly recommend maintaining the rest of your body’s fitness with regular exercise while you rehabilitate your elbow. Maintaining general cardiovascular fitness can be done with lower extremity fitness activities such as walking or using a stationary bike or stepper machine. Weights for your other arm or lower extremities can also be done but you may require a friend to assist you in the gym as lifting any weight, even just to prepare a machine could be detrimental to your elbow rehabilitation and should not be undertaken until your physiotherapist deems it appropriate.
 The elbow joint is injured less often than many other joints in the body. The most common injuries of the elbow joint are fractures and dislocations. Fortunately most elbow injuries tend to heal fairly well at the time of injury.
The elbow joint is injured less often than many other joints in the body. The most common injuries of the elbow joint are fractures and dislocations. Fortunately most elbow injuries tend to heal fairly well at the time of injury. The elbow joint is made up of three bones: the humerus bone of the upper arm, and the ulna and radius bones of the forearm.
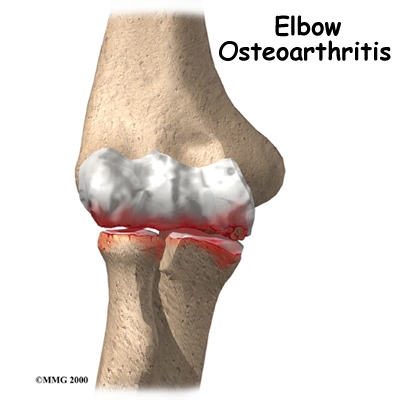
The elbow joint is made up of three bones: the humerus bone of the upper arm, and the ulna and radius bones of the forearm. OA is caused by degeneration of the articular cartilage of a joint. Degeneration is wear that happens over time. Doctors use the term degenerative arthritis to describe the wear and tear of a joint over many years. Degenerative arthritis is another term for OA. Some doctors use the term degenerative arthrosis. Arthrosis means that the joint is wearing out.
OA is caused by degeneration of the articular cartilage of a joint. Degeneration is wear that happens over time. Doctors use the term degenerative arthritis to describe the wear and tear of a joint over many years. Degenerative arthritis is another term for OA. Some doctors use the term degenerative arthrosis. Arthrosis means that the joint is wearing out. Unfortunately the human body does not do a good job of repairing these holes in the cartilage surface of joints. The holes fill up with scar tissue. Scar tissue is not as slick or rubbery as the articular cartilage so the joint mechanics suffer.
Unfortunately the human body does not do a good job of repairing these holes in the cartilage surface of joints. The holes fill up with scar tissue. Scar tissue is not as slick or rubbery as the articular cartilage so the joint mechanics suffer. In order to help determine if OA is present you will probably need to get standard X-rays. X-rays are usually the best way to see what is happening with your bones if OA is suspected. X-rays can help your health care professional assess the damage and track how your joint changes over time. X-rays can also help your health care professional see how many bone spurs are present and if there are any loose bodies in the joint. X-rays also show the size of the joint space and how much articular cartilage is left.
In order to help determine if OA is present you will probably need to get standard X-rays. X-rays are usually the best way to see what is happening with your bones if OA is suspected. X-rays can help your health care professional assess the damage and track how your joint changes over time. X-rays can also help your health care professional see how many bone spurs are present and if there are any loose bodies in the joint. X-rays also show the size of the joint space and how much articular cartilage is left.
 If you are in an early stage of OA, your doctor may recommend arthroscopic debridement. Other names for this procedure include arthroscopic ulnohumeral arthroplasty or osteocapsular arthroplasty.
If you are in an early stage of OA, your doctor may recommend arthroscopic debridement. Other names for this procedure include arthroscopic ulnohumeral arthroplasty or osteocapsular arthroplasty. Before the invention of high-quality artificial joints, surgeons used many techniques to keep the bone surfaces of arthritic joints from rubbing against each other. One of these techniques is distraction interposition arthroplasty. This procedure involves placing a piece of tendon or fascia between the bony surfaces of the elbow joint. Fascia is a connective tissue, similar to tendon that lies in a flat sheet. It covers the muscles and acts as a divider between different compartments of the body.
Before the invention of high-quality artificial joints, surgeons used many techniques to keep the bone surfaces of arthritic joints from rubbing against each other. One of these techniques is distraction interposition arthroplasty. This procedure involves placing a piece of tendon or fascia between the bony surfaces of the elbow joint. Fascia is a connective tissue, similar to tendon that lies in a flat sheet. It covers the muscles and acts as a divider between different compartments of the body. A fusion surgery (also called arthrodesis) eliminates pain by making the bones of the joint grow together, or fuse, into one solid bone. Fusions were very common before the invention of artificial joints. Even today, joint fusions are commonly used in many different joints to get rid of the pain of arthritis.
A fusion surgery (also called arthrodesis) eliminates pain by making the bones of the joint grow together, or fuse, into one solid bone. Fusions were very common before the invention of artificial joints. Even today, joint fusions are commonly used in many different joints to get rid of the pain of arthritis. Elbow joint replacement, however, is a good choice for patients who need improved motion rather than strength. Older patients who don't need as much strength will probably prefer the results of elbow replacement surgery, however, they must be willing to accept low levels of activity involving the elbow. Patients with advanced rheumatoid arthritis are also good candidates for TEA.
Elbow joint replacement, however, is a good choice for patients who need improved motion rather than strength. Older patients who don't need as much strength will probably prefer the results of elbow replacement surgery, however, they must be willing to accept low levels of activity involving the elbow. Patients with advanced rheumatoid arthritis are also good candidates for TEA.